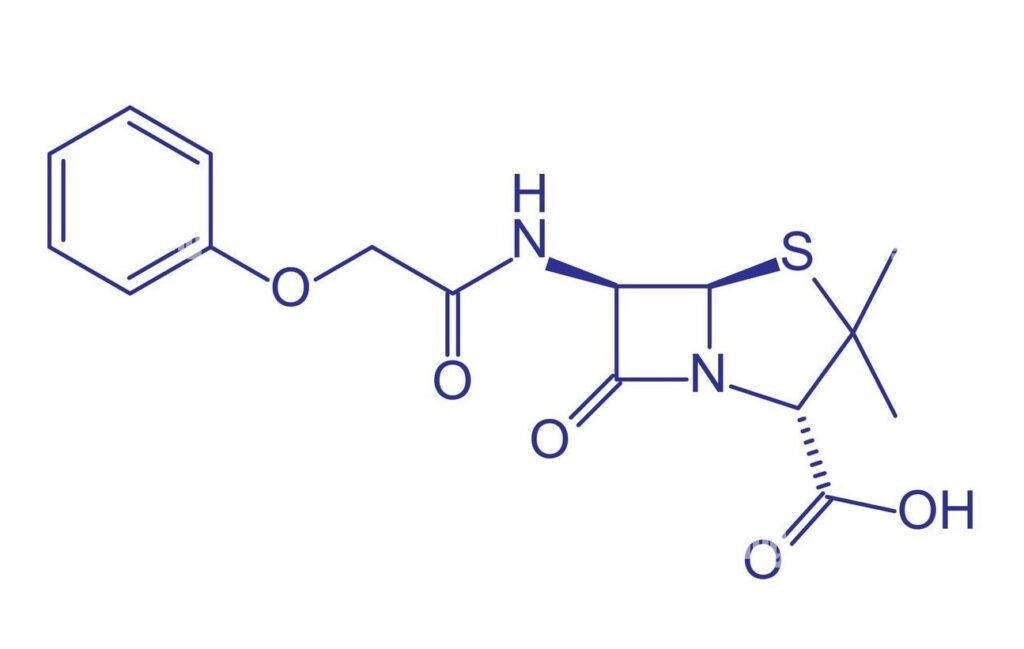
Phenoxymethylpenicillin is an essential penicillin antibiotic, widely used to treat various bacterial infections and prevent recurrent illnesses. This comprehensive article covers every aspect of the drug, including history, uses, mechanism, side effects, societal impact, and recent developments. Detailed FAQs are included for maximum clarity.
Introduction to Phenoxymethylpenicillin
Phenoxymethylpenicillin, also known as Penicillin V or Penicillin VK, is a time-tested antibiotic from the beta-lactam family. Unlike many antibiotics, it is acid-stable and can be safely taken as tablets or liquid, making it suitable for oral administration. Primarily, it targets Gram-positive bacteria, proving highly effective for treating infections of the throat, ear, chest, skin, and teeth, among others.
Table: Key Facts
Historical Background
The story of phenoxymethylpenicillin begins with the initial discovery of penicillin in 1928 by Alexander Fleming. While Fleming’s original discovery focused on benzylpenicillin, it wasn’t until 1948 that Eli Lilly first synthesised phenoxymethylpenicillin. Its oral administration advantage was leveraged in the 1950s, when researchers discovered its acid stability, a breakthrough that revolutionised outpatient treatment for mild to moderate infections. The Austrian firm Biochemie further refined its commercial production in the early 1950s, realising its ability to withstand stomach acid. Today, it sits on the World Health Organisation’s List of Essential Medicines and remains available in generic form worldwide.
Medical Uses and Indications
Phenoxymethylpenicillin’s versatility has cemented its place in medicine. Its spectrum includes:
- Treatment of Streptococcus pyogenes infections: strep throat, tonsillitis, pharyngitis, and certain skin infections.
- Management of mild anthrax cases and early Lyme disease (especially in pregnant women and young children).
- Prevention of recurrent rheumatic fever and post-splenectomy infections.
- Dental uses: initial therapy for dental abscesses and severe gingivitis.
- Prophylaxis in children with sickle cell disease to prevent blood infections.
It is important to note that phenoxymethylpenicillin is less effective than benzylpenicillin against Gram-negative bacteria and is not useful against beta-lactamase producers like many Staphylococci.
Mechanism of Action
As a beta-lactam antibiotic, phenoxymethylpenicillin disrupts bacterial cell wall synthesis. It binds to penicillin-binding proteins (PBPs) within the cell wall, blocking peptidoglycan biosynthesis. This weakens the bacterial wall, causing cell death. The main predictor of its effectiveness is maintaining blood concentrations above the minimum inhibitory concentration for the target bacteria.
Dosage and Administration
Phenoxymethylpenicillin is typically prescribed as tablets or oral solutions, taken four times daily. Dosages are calibrated according to age, weight, and the severity of infection. In most cases, patients begin to feel better within days. The medicine is only available with a prescription and should be taken after food to minimise stomach upset.
Side Effects and Safety
Common side effects of phenoxymethylpenicillin include:
- Nausea and vomiting
- Diarrhoea and mild stomach pain
- Allergic reactions, ranging from mild rash to severe anaphylaxis
- Rare effects such as a black hairy tongue or constipation
Individuals with a history of penicillin allergy must avoid this drug. Its safety profile supports use during pregnancy and breastfeeding, with physician guidance. Patients should always disclose other medical conditions (especially kidney or liver issues) and medication histories to prevent adverse interactions.
Resistance and Limitations
Resistance to phenoxymethylpenicillin arises primarily from beta-lactamase (penicillinase) production, which inactivates the drug. Some bacteria possess altered PBPs that lower drug affinity, which can also confer resistance. Therefore, microbiological sensitivity testing is crucial for cases other than Streptococcus pyogenes, which remains uniformly sensitive.
Phenoxymethylpenicillin in Modern Healthcare
In recent years, phenoxymethylpenicillin has remained widely prescribed, ranking among the top antibiotics in prescription frequency. Its generic availability ensures affordability and accessibility for millions globally.
The antibiotic has also found renewed favour as a first-line agent in dental and certain pediatric infections due to its narrow spectrum, minimising the risk of antibiotic resistance development. However, supply chain challenges do emerge: in late 2022 and early 2023, several countries, including the UK, experienced shortages due to surging demand during outbreaks of strep throat among children.
Recent News and Supply Issues
- In December 2022, the UK instituted Serious Shortage Protocols (SSPs) for phenoxymethylpenicillin, permitting pharmacists to dispense alternative formulations to meet demand stemming from increased Strep A infections.
- In 2024, Kent Pharma UK issued a precautionary recall of a batch of phenoxymethylpenicillin oral solution following quality concerns in stability studies.
- Despite supply challenges, authorities assure the overall adequacy of alternatives and adjusted dispensing to safeguard patient care.
Societal and Cultural Impact
Phenoxymethylpenicillin is known internationally by various names: Penicillin V, Penicillin VK (potassium salt form), and within professional circles as “V” for its “confidential” origins (from the German ‘Vertraulich’). Its enduring use and safety profile have made it a mainstay in preventive medicine and primary care.
Detailed FAQs About Phenoxymethylpenicillin
What is phenoxymethylpenicillin used for?
Phenoxymethylpenicillin treats bacterial infections of the throat, ear, chest, skin, and teeth, and is employed for preventing rheumatic fever, post-splenectomy infections, and blood infections in sickle cell disease.
How is phenoxymethylpenicillin taken?
Phenoxymethylpenicillin is taken orally as tablets or solutions, typically four times a day, with doctor-directed dosing based on age and severity.
Is phenoxymethylpenicillin safe in pregnancy or breastfeeding?
It is generally considered safe for use during pregnancy or while breastfeeding, but should only be used under medical supervision.
What are the main side effects?
Side effects include nausea, diarrhoea, rash, and rare allergic reactions. Any prior allergy to penicillin-class antibiotics excludes its use.
Can phenoxymethylpenicillin treat viral infections?
No. Phenoxymethylpenicillin is strictly for bacterial infections and is ineffective against viruses such as the flu or common cold.
Why are shortages sometimes reported?
Occasional shortages result from spikes in demand (e.g., during outbreaks of strep throat) or manufacturing and quality control issues, prompting temporary alternative dispensing protocols.
How does resistance occur?
Resistance arises primarily when bacteria produce beta-lactamase enzymes that deactivate the antibiotic or alter penicillin-binding proteins.
Is alcohol allowed during treatment?
Alcohol does not interfere with phenoxymethylpenicillin and may be consumed in moderation while on treatment.
How do you know if it is working?
Most patients feel improvement within a few days. Symptoms persisting or worsening may indicate resistance or an improper diagnosis, prompting further medical review.
Is phenoxymethylpenicillin still commonly prescribed?
Yes. It remains a commonly dispensed antibiotic worldwide for various community-acquired bacterial infections.